Last updated on June 15th, 2023
Dysphagia affects about 50% of long-term care patients and can lead to an increased risk of dehydration and malnutrition. So, what is Dysphagia? The Centers for Medicare & Medicaid Services (CMS) defines Dysphagia as “a swallowing disorder that may be due to various neurological, structural, and cognitive deficits.”
How is Dysphagia Treated in the Elderly?
Many Dysphagia patients are fed texture-modified diets, like thickened liquids, to decrease the risk of aspiration. It’s important for staff at senior living communities to understand what Dysphagia is and how to provide the right food for these patients because the Academy of Nutrition and Dietetics announced that in October 2021, the International Dysphagia Diet Standardization Initiative (IDDSI) will be the only texture-modified diet recognized in the Academy’s Nutrition Care Manual (NCM).
This change is being made to standardize food production and fluid thickness across all healthcare facilities to give Dysphagia patients the best and most consistent care possible. IDDSI provides precise descriptions for preparing texture-modified diets. It also offers training resources on its website so all healthcare providers can understand how to prepare foods for Dysphagia patients safely.
If your community currently uses the Academy’s NCM, your team will need to change your Dysphagia dining program by October 2021.
There are also a few F-Tags that are related to Dysphagia treatment. Your state and CMS use F-Tags to ensure that your community provides safe, quality care to residents. You may be evaluated on your Dysphagia dining program when food surveyors assess your kitchens for compliance with the following F tags:
- F805: Each resident receives food, and the facility provides food prepared in a form designed to meet individual needs.
- F808: To assure that residents receive and consume foods in the appropriate form and/or the appropriate nutritive content as prescribed by a physician and/or assessed by the interdisciplinary team to support the resident’s treatment plan according to their goals preferences.
- F810: The facility must provide special eating equipment and utensils for residents who need them and appropriate assistance to ensure that the resident can use the assistive devices when consuming meals and snacks.
- F811: To ensure that residents are assessed for appropriateness for a feeding assistant program, receive services as per their plan of care, and feeding assistants are trained and supervised. The use of paid feeding assistants is intended to supplement certified nurse aides, not substitute for nurse aides or licensed nursing staff.
The Problem with Many Texture-Modified Diets for Dysphagia
Many textured-modified diets can be unappealing to patients and lead to a lower quality of life. Residents often find the prescribed modified or pureed foods to be unappetizing, which is why they eat less of them.
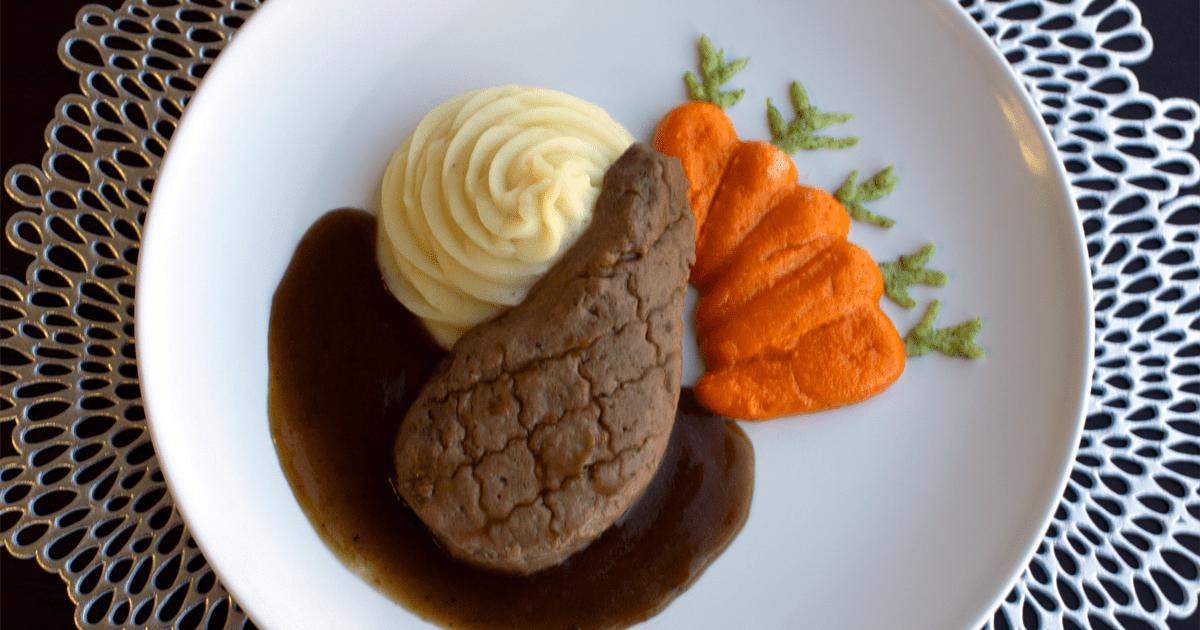
Research shows that food presentation alone can boost appetites, and nicely plated foods are perceived to taste better. That’s why Culinary Services Group created the Appeal Premium Dining Program for the senior living communities we work with. At Culinary Services Group, we have a food-first philosophy, meaning we always offer real food first. All of our food, regardless of texture, is made from scratch using the freshest ingredients possible.
The Appeal Program focuses on artfully shaping and presenting puréed foods into familiar and comforting meals for patients with Dysphagia. The Appeal Program meal plan includes the same proteins that are a community’s daily menu. Puréed diet items are passed through mechanical strainers to ensure that residents don’t receive any lumps or pieces after proteins are processed. Then, using molds, piping techniques, and layering, our team creates plates that look and taste great.
For example, if lunch for the day includes a roast beef and cheddar sandwich, German potato salad, a side salad, and a pudding parfait, the Appeal modification would be a roast beef (puréed & molded) with cheese sauce, puréed potato salad (piped or quenelle scooped), a puréed side salad, and a pudding parfait.
Appeal offers meal options and opportunities to residents at all levels of the IDDSI spectrum of modified eating. When communities implement this program, they see increased meal consumption, reduced weight loss and malnutrition, and an overall healthier population.
How to Implement the Appeal Program for Dysphagia Patients
When communities select the Appeal Program, the Culinary Services Group team supports them with necessary implementation resources. A Registered Dietitian and Food Service Director will meet with your Area Manager, Sr. Director of Nutrition, and Sr. Director of Culinary to assess how the Appeal program will work in your community. We’ll assess your current cycle menu to determine which changes and substitutions will need to be made. We’ll also give your team a production manual and proper supplements, thickeners, and molds.
Our Registered Dietitian will partner with your clinical leadership to determine the needs of individual residents before enrollment and how best to document diet modifications. Our dietitians and chefs prepare a customized menu specific to the community with a wide variety of foods that fit within the program’s guidelines and take into consideration resident preferences. We will also provide continuous training and support to your dining team.
Contact us here to learn more about how the Appeal Premium Program can help you provide healthy, great-tasting meals to residents with Dysphagia.